Introduction
Tinea corporis, commonly known as ringworm of the body, is a superficial fungal infection of the skin caused by dermatophyte fungi. Despite the name, it is not caused by worms. It typically appears as round or ring-shaped, itchy, red patches with clearer centers.
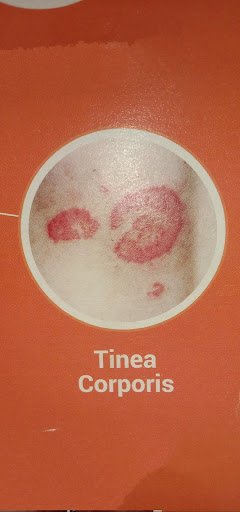

TINEA CORPORIS
Causes
Tinea corporis is caused by dermatophyte fungi, mainly:
- Trichophyton
- Microsporum
- Epidermophyton
The infection spreads through:
- Direct skin-to-skin contact
- Contact with infected animals (cats, dogs, cattle)
- Sharing contaminated objects like towels, clothes, bedding, combs
- Touching infected soil (rare)
Signs and Symptoms
Common symptoms include:
- Circular or ring-shaped red patches
- Raised, scaly borders
- Central clearing (normal-looking skin in the middle)
- Itching or burning sensation
- Dry, flaky skin
- Sometimes blisters or oozing in severe cases
The lesions can appear on the:
- Arms
- Legs
- Chest
- Back
- Face
Who Is at Risk?
People more likely to develop tinea corporis:
- Children
- Athletes (especially wrestlers)
- People living in hot and humid climates
- Diabetics
- Immunocompromised individuals
- People with poor hygiene
- Those using tight or sweaty clothing for long periods
Is Tinea Corporis Contagious?
✅ Yes, it is highly contagious. It can spread through direct or indirect contact until it is properly treated.
Diagnosis
Usually diagnosed clinically by a doctor. Sometimes the following may be done:
- KOH (potassium hydroxide) skin scraping test
- Fungal culture (in doubtful cases)
- Dermoscopy
- Wood’s lamp examination (for some species)
Treatment of Tinea Corporis
1. Topical Antifungal Creams (for mild cases)
Apply 2 times daily for 2–4 weeks:
- Clotrimazole
- Terbinafine
- Miconazole
- Ketoconazole
- Luliconazole
2. Oral Antifungal Medicines (for extensive or severe cases)
Prescribed by a doctor:
- Terbinafine
- Itraconazole
- Fluconazole
- Griseofulvin (less commonly used now)
⚠️ NOTE:-
Never use steroid combination creams (like betnovate-N, quadriderm, etc.) without doctor advice, as they worsen fungal infections.
Home Remedies
- Keep the affected area clean and dry
- Wear loose, cotton clothes
- Avoid sharing towels, clothes, and bedding
- Wash clothes in hot water
- Dry skin properly after bathing
- Avoid scratching
Prevention
- Maintain personal hygiene
- Keep skin dry, especially skin folds
- Use separate towels
- Avoid walking barefoot in public places
- Treat infected pets if they are a source
Difference Between Tinea Corporis and Other Ringworm Types
| Type | Area Affected |
| Tinea corporis | Body (arms, legs, trunk) |
| Tinea cruris | Groin |
| Tinea pedis | Feet (athlete’s foot) |
| Tinea capitis | Scalp |
| Tinea faciei | Face |
Frequently Asked Questions (FAQ)
Q1. Is tinea corporis dangerous?
No, it is not dangerous but can spread and cause discomfort if untreated.
Q2. How long does it take to cure?
Mild cases: 2–4 weeks with proper treatment.
Severe cases may take longer.
Q3. Can it come back after treatment?
Yes, if hygiene is poor or treatment is stopped early.
Q4. Can home remedies cure it?
Home remedies may give temporary relief, but antifungal medicines are necessary for complete cure.
Q5. Should I stop using steroid creams?
Yes, unless advised by a doctor. Steroids worsen fungal infections.
Conclusion
Tinea corporis is a common and easily treatable fungal skin infection. Early diagnosis, proper antifungal treatment, and good hygiene can prevent its spread and recurrence.